Malaria vaccine shows promise
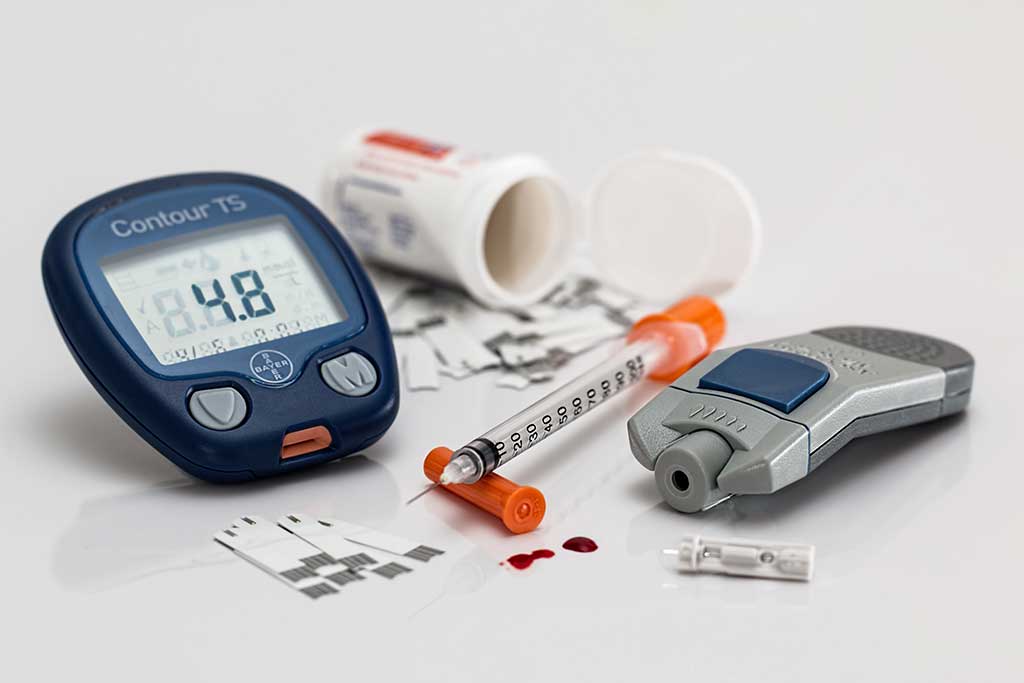
Medication
The Independent reported today that a vaccine for malaria could be available within five years. It said two extensive trials of a vaccine called RTS,S were carried
The Independent reported today that a vaccine for malaria could be available within five years. It said two extensive trials of a vaccine called RTS,S were carried out in Tanzania and Kenya. The studies found that the vaccine can be given as part of an immunisation programme without compromising the other vaccines. It also reduced malaria infection by up to 65% in children under one year, and by 53% in children aged five to 17 months.
These two well-designed studies are the most advanced trials of antimalarial vaccines so far, and are important steps in the fight against malaria. They have demonstrated that the vaccine currently reduces the risk of developing malaria, but does not completely prevent it.
Further studies will need to be carried out to confirm these findings, and the trials extended to areas with higher levels of malaria infection. The vaccination targets the most severe form of malaria caused by the parasite Plasmodium falciparum and so would be unlikely to offer any protection against the other types of malaria: Plasmodium vivax, Plasmodium ovale and Plasmodium malariae.
Where did the story come from?
The newspaper reports are based on two studies published in the peer-reviewed journal, New England Journal of Medicine. The first study took place in Kenya and Tanzania, the first author of which was Dr Philip Bejon from the Kenya Medical Research Institute. The second study took place in Tanzania and the first author was Dr Salim Abdulla from the Ifakara Health Institute in Tanzania. Both studies involved scientists from research centres around the world.
The studies were funded by the PATH Malaria Vaccine Initiative and the manufacturers of the vaccine, GlaxoSmithKline Biologicals.
What kind of scientific study was this?
Both studies are double blind randomised controlled trials that looked at the efficacy of the RTS,S vaccine at preventing malaria in infants and children. The vaccine targets the Plasmodium falciparum parasite that causes malaria. The vaccines used in the two studies were formulated in slightly different ways, using two different “adjuvants”. Adjuvants are chemicals mixed with the vaccine to enhance its ability to promote an immune response. The Tanzanian study used the AS02D adjuvant while the Kenyan study used the AS01E adjuvant.
Tanzanian study
The main aim of the Tanzanian study was to look at the safety of these vaccines and to show that if they were given with other childhood vaccines (the Expanded Program on Immunization, or EPI, vaccinations) that they would not make the other vaccines less effective. A secondary aim of the study was to see if the vaccine reduced the proportion of children who had malaria that lead to symptoms.
The researchers enrolled 340 infants (younger than eight weeks of age) and randomly assigned them to receive either the RTS,S/AS02D vaccine or a hepatitis B vaccine (control). The vaccines were given by injection at 8, 12, and 16 weeks of age, along with vaccinations against diphtheria, tetanus, whooping cough, and influenza (EPI vaccinations). Two weeks before the final dose of the vaccine, the infants were given a course of the antimalarial drugs artemether-lumefantrine (six doses given over three days) to clear any pre-existing P. falciparum infections. The infants were monitored for side effects for an hour after each vaccination, were visited at home once a day for the next six days, and then once a month for the next nine months.
At the last vaccination the infants were tested for infection, and any who did have infections received further vaccination and were only included in the safety analyses, but not the immunity or malaria analyses parts of the study. The infants’ immune response to the EPI vaccinations was tested at the beginning of the study (when little immunity would be expected) and at one month after the second and third vaccinations.
Before the study began, the researchers decided that the antimalarial vaccine would be judged to be “inferior” if it reduced antibody reactions to the EPI vaccines by a set amount (over 10% for the diphtheria, tetanus, influenza or hepatitis B, or over 1.5 times for the whooping cough).
The infants were monitored for symptoms of clinical malaria in the six months after the final vaccination and those showing symptoms were tested for malarial infection.
The researchers then compared the antimalaria vaccine and control groups in terms of safety, immune response and the proportion of infants who developed clinical malaria. The analyses of clinical malaria were adjusted for the length of time each infant remained in the study, and also which village they lived in and their distance from the health facility.
Kenyan study
The main aim of the Kenyan study was to look at whether the RTS,S/AS01E vaccine reduced the risk of malaria. Previous studies had shown a 30% reduction of clinical malaria in children between the ages of one and four using the RTS,S vaccine with the AS02E adjuvant. The researchers wanted to see if the AS01E adjuvant would improve on these rates.
The researchers enrolled 894 children aged between five and 17 months of age and randomly assigned them to receive either the RTS,S/AS01E vaccine or an anti-rabies vaccine (control). Vaccinations were given once a month for three months and monitoring for malaria started 2.5 months after the first vaccination and carried on for an average of about eight months. Children were defined as having clinical malaria if they had a fever, and if their blood tests showed over 2,500 P. falciparum parasites per microlitre of blood.
What were the results of the study?
In the Tanzanian study, 18% of the infants (31 out of 170) who received the RTS,S/AS02D vaccine experienced one or more serious adverse effects (mostly pneumonia), compared with 25% of the infants (42 out of 170) who received the control hepatitis B vaccination. The antimalarial vaccine did not affect how well the EPI vaccines worked.
About 99% of the children who received the antimalarial vaccine showed an antibody response to the vaccine. Over the period from two weeks to seven months after the final vaccination, 146 infants in the antimalarial vaccine group and 151 infants in the control group were monitored for clinical malaria and were eligible for analysis. Eight children in the antimalarial vaccine group developed at least one episode of malarial infection compared with 20 in the control group. After adjustments, this meant that the vaccine reduced malarial infections by 65%.
In the Kenyan study, 809 children completed the study according to the protocol and were included in the analyses. Thirty-two of the 402 children in the antimalarial vaccine group developed clinical malaria compared to 66 of the 407 children in the control group. After adjustments, this meant that the vaccine reduced malarial infections by 56%. The researchers got similar results if they included all 894 children in their analyses. There were fewer adverse effects of the antimalarial vaccine than the control vaccine.
What interpretations did the researchers draw from these results?
In the Tanzanian study, the researchers concluded that the RTS,S/AS02D vaccine had a “promising safety profile” and “did not interfere with the immunologic response to co-administered EPI [vaccinations]”, as well as reducing malarial infections.
In the Kenyan study, the researchers concluded that the RTS,S/AS01E vaccine “shows promise as a candidate malaria vaccine”.
What does the NHS Knowledge Service make of this study?
These two studies both show promising results in the prevention of malaria in infants and children. The finding that the RTS,S/AS02D vaccine could be given alongside other childhood vaccinations without reducing their efficacy is particularly important.
Further larger scale trials will be needed to confirm these findings. In particular, as the levels of malarial infections in these two regions were relatively low, the vaccines will need to be tested in areas with higher infection levels.
These two studies demonstrated that the vaccine reduced the risk of developing malaria, but did not cause complete prevention; therefore, it should not be assumed that a vaccine “just four years away” could eradicate malaria.
Additionally, the vaccination only targets the most severe form of malaria caused by the parasite Plasmodium falciparum . It is unlikely that the vaccine would offer any protection against the other types of malaria: Plasmodium vivax, Plasmodium ovale and Plasmodium malariae.
Sir Muir Gray adds...
Very important, very promising.






 Subscribe
Subscribe Ask the doctor
Ask the doctor Rate this article
Rate this article Find products
Find products